- ABSTRACT
The objective of this clinical case is to demonstrate the correction of an anterior open bite with a narrow maxilla in an adult patient taking into account the anterior rotational response of the mandible.
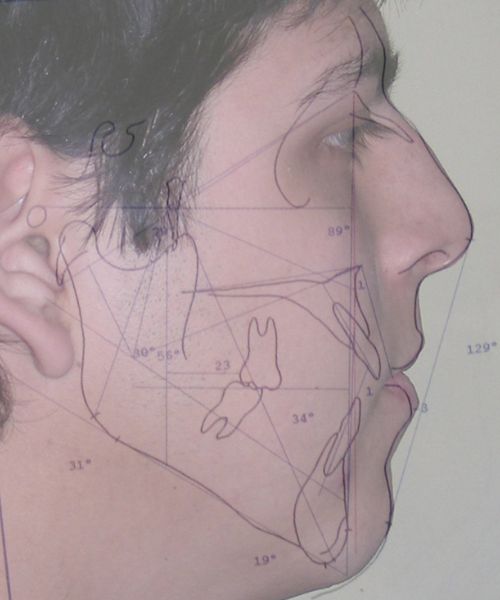
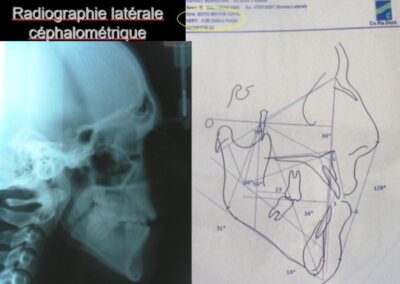
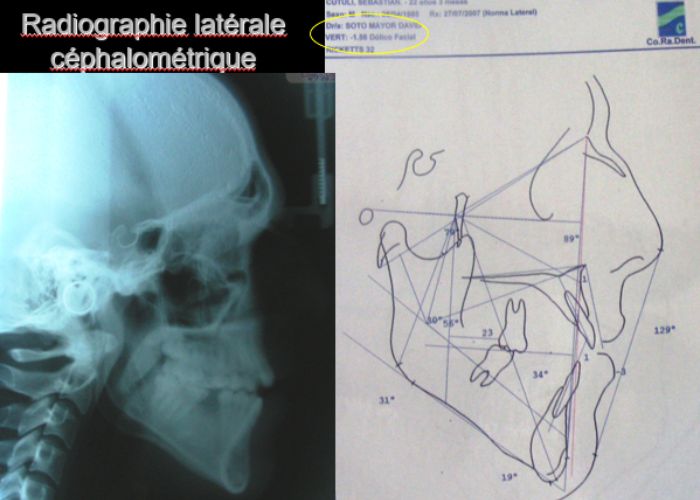
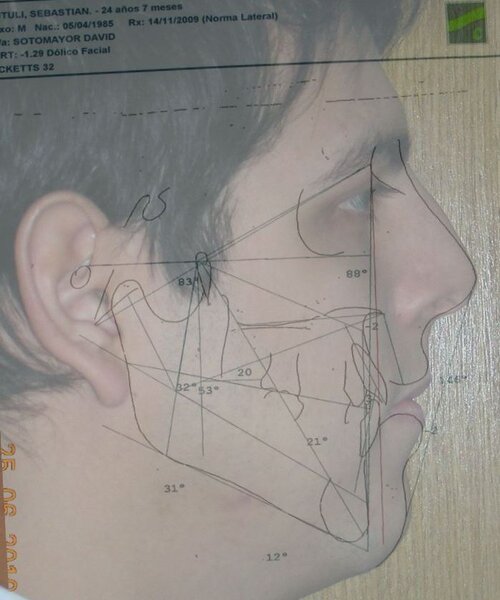
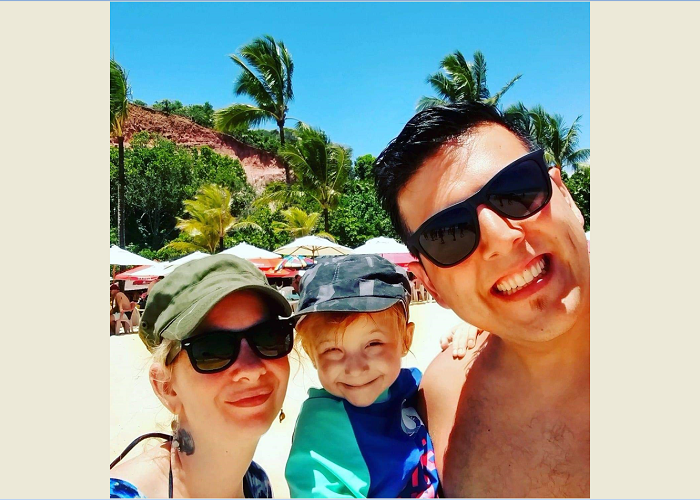
22-year-old male patient who comes to my Orthodontic Clinic when asking his reason for consultation: « I don’t like my smile and when I speak I tend to expel saliva Ahh! and I want to be able to bite an apple, laughs » he responds with good humor. On extraoral clinical examination, a face is seen vertically with the lower third enlarged. Its profile is slightly convex with poor chin projection. Intraorally evidence of anterior open bite in addition to bilateral crossed occlusion. Cephalometrically, a vertical disproportion was confirmed, which coincides with a skeletal-based open bite. The proposed treatment was orthodontic-surgical, Bimaxillary. Lefort I impaction plus bilateral mandibular ramus osteotomy (BSSO) with possible genioplasty, to which the patient rejected, taking into consideration only orthodontic treatment with anchorage aids (microscrews or TADs). In this way, the commitment treatment begins beyond the limitations imposed by the patient’s skeletal reality.
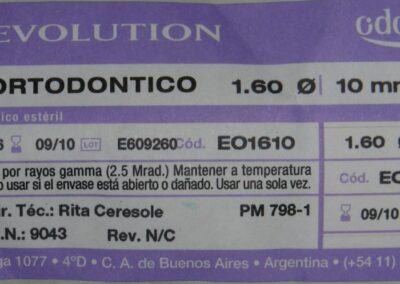
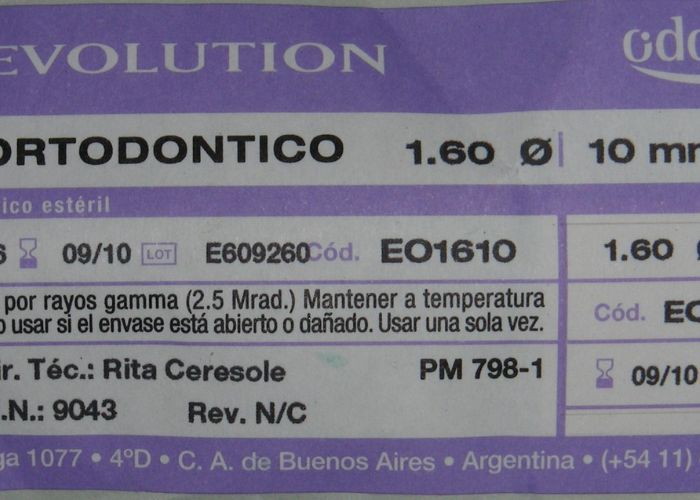
Key words: Cross-Bite EPR – Hyrax Skeletal Open-Bite orthognathic surgery TADs
- INTRODUCTION
Proffit defines overbite as the overlap of the incisors in which the incisal edges of the lower teeth are in contact with the incisal and middle thirds of the palatal surface of the upper incisors, slightly below the cingulum. In open bites, vertical overlap does not occur.1 This condition may occur in a single tooth or in a group of teeth.2 Its severity varies from an almost edge to edge relationship up to a severe open bite.3 Open bite incidence varies depending on age and ethnic group being more common in African and Afro-Caribbean populations.4
Although the majority of patients with anterior open bite seek treatment only for aesthetic reasons, several problems may occur such as lack of anterior and canine guidance, difficulty for tearing food, language problems (lisp) and temporomandibular disorders among others.2,4,5
Anterior open bite may be divided into two categories:
Dental open bite: the vertical skeletal pattern does not contribute to the malocclusion and is usually present in the anterior region, from canine to canine; the maxillary incisors are protruded and proclined and commonly results from a habit.
Skeletal open bite: the skeletal pattern does have an influence in the malocclusion and is characterized by an elongation of the lower third of the face, rotation of the mandible in a clockwise direction, a hyperdivergent growth pattern and occlusal contacts only in molars.2,3,6
Development of anterior open bite is the result of the interaction of several factors such as: skeletal disharmonies in which an excessive vertical grow this present, lack of muscular balance, habits such as digital sucking, abnormal function of the tongue, airway obstruction or iatrogenic treatments.3,5–7
The majority of orthodontists are consistent with the fact that anterior open bite is one of the most difficult malocclusions to treat and the one with the largest percentage of relapse even when the patient is treated with orthognathic surgery. Identifying the etiology of the problem provides a greater percentage of success at the end of treatment.2,5,7–11
The literature describes different treatment modalities with the purpose of reducing relapse including miofunctional appliances, fixed appliances, lingual cribs, elastics, wires, molar intrusion, extrusion of the upper anterior teeth, aligners with elastics, orthognathic surgery, extractions, partial glossectomy or orofacial miofunctional therapy.10,11
Mizrahi described four alternatives: miofunctional therapy, orthodontic treatment with fixed or removable appliances, surgical treatment or a combination of the above mentioned.12
For Ngan, by using simple techniques in which the etiologic factors are eliminated the bite is closed through the normal eruptive process.6
Lopez-Gavito reported that more than 35 per cent of anterior open bites treated with conventional appliances relapsed 3mm or more at 10 years post-retention.13
Phelan et al found favorable effects in patients who underwent maxillary expansion and in whom a high-pull chincap was used at the peak of mandibular growth. They also recommended not perform treatment in early stages since it was best to wait until the pubertal stage.4
Pearson reported that the use of a chincap may reduce the mandibular plane angle and that this decrease prevents an increase in facial height and an over-eruption of the posterior teeth but that low reliability rates were presented.14,15
Various researchers conclude that tongue position and activity are the reasons why it is difficult to achieve long-term stability. It has been found that orofacial miofunctional therapy combined with orthodontics significantly reduces the possibility of relapse.5,10
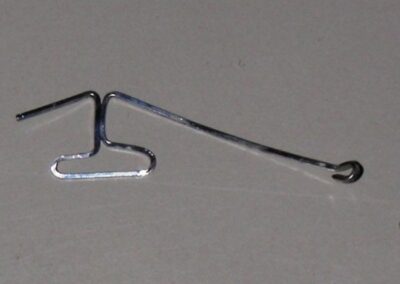
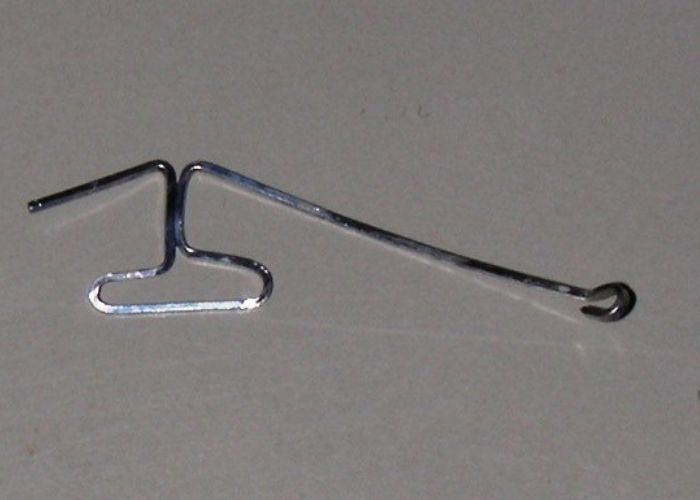
Justus suggests modifying tongue position through the use of spurs due to the fact that patients with open bite most of the time rest the tongue over the incisors. In his research Dr. Justus found that spurs are an excellent choice for both bite closure and stability.5
- FULL CASE
Extraoral Pictures
Upon facial analysis, the patient showed a dolichofacial biotype with an increased lower middle facial third; The width of the mouth coincides with the interiris line, the nasal width coincides with the inner edge of the eye, Lip competence is achieved by tension of the mentalis muscle. The most striking aspect is the adenoid facies that anticipates his respiratory condition. We find slightly convex profile.
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
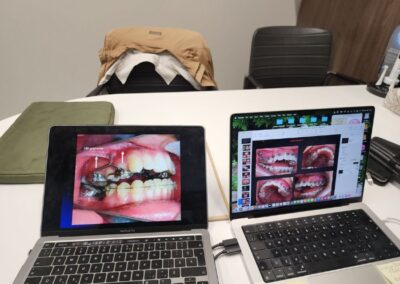
Intraoral Pictures
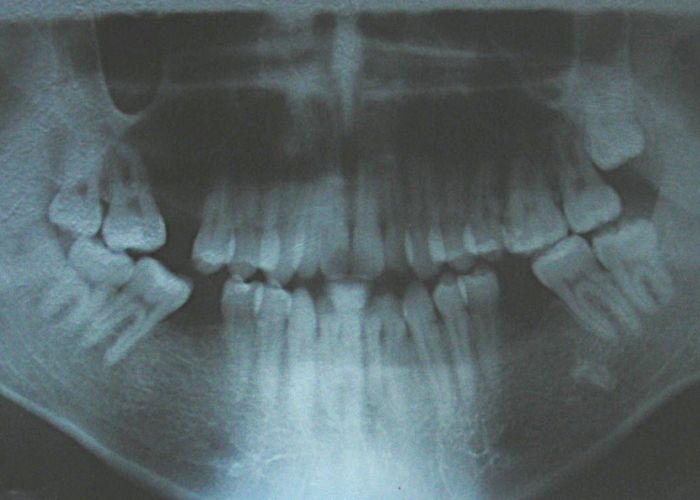
During the intraoral examination, an anterior open bite was observed in addition to bilateral posterior crossed occlusion, the lower dental midline deviated from the upper one by 3mm to the left (projection), an overbite of -7mm, and an unclassified molar relationship due to the absence of the 1st, canine class molar. II (projection), Triangular-shaped upper arch with moderate crowding. Ovoid lower arch with moderate crowding.
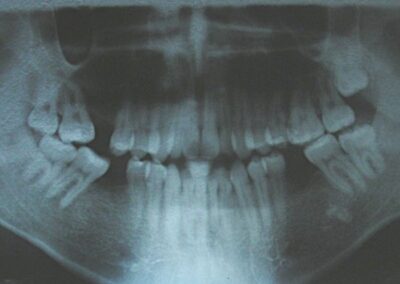
Absence of 16, 36 and 46.
In the panoramic x-ray we see the presence of upper wisdom molars. No alteration at the roots level, TMJ , maxillary or mandibular bone level.
Your Title Goes Here
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
cephalometric analysis and treatment plan
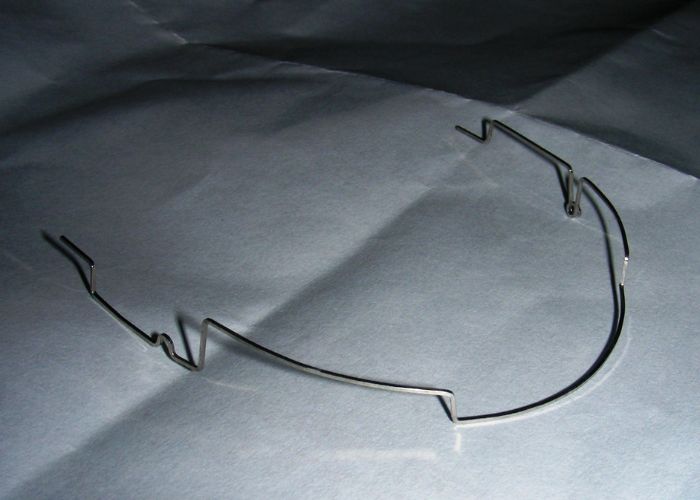
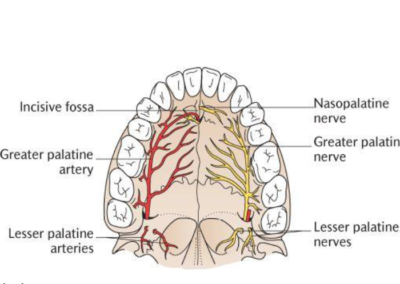
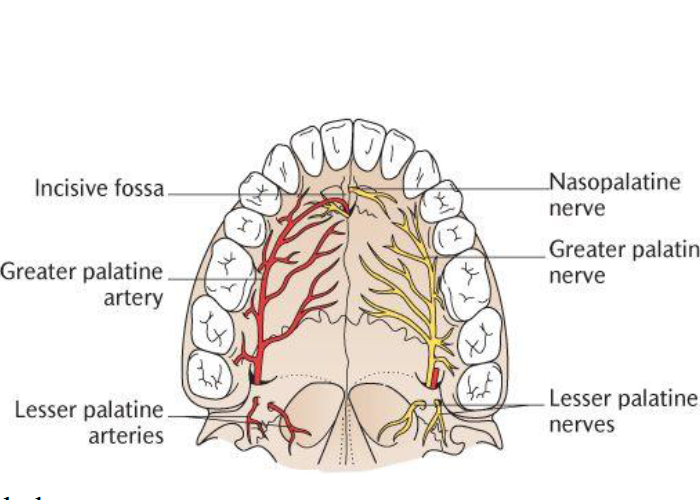
1. Perform palatal expansion.
2. Perform intrusion of the upper posterior sectors.
3. Perform mesialization of the lower posterior sectors.
4. Obtain anterior guidance (incisors and canines)
5. Achieve a stable seat on the premolars.
6. Overtreatment
7. Reference to speech therapy
8.Containment. Maintain a permanent stable result.
under construction
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
Hierarchical treatment sequence
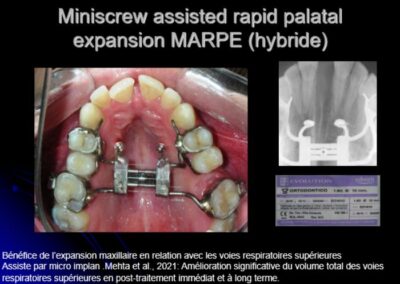
Benefit of maxillary expansion in relation to the upper respiratory tract Assisted by micro implan. Mehta et al., 2021: Significant improvement in total upper airway volume in immediate and long-term post-treatment.
Your Title Goes Here
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.







Your Title Goes Here
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
Your Title Goes Here
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
Your Title Goes Here
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
Your Title Goes Here
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
Your Title Goes Here
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
Your Title Goes Here
Your content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
- CONCLUSIONS
REFERENCES
Am J Orthod Dentofacial Orthop., 131 (2007), pp. 670-678
Dent Update, 30 (2003), pp. 235-241
Am J Orthod Dentofacial Orthop., 145 (2014), pp. 28-35
Pediatr Dent., 19 (1997), pp. 91-98
Am J Orthod Dentofacial Orthop., 143 (2013), pp. 412-420
Angle Orthod., 78 (2008), pp. 415-420
Am J Orthod Dentofacial Orthop., 138 (2010), pp. 14.e1-14.e7
Am J Orthod Dentofacial Orthop., 137 (2010), pp. 605-614
World J Orthod., 10 (2009), pp. 130-134
Br J Orthod., 5 (1978), pp. 21-27
Am J Orthod., 87 (1985), pp. 175-186
Am J Orthod Dentofacial Orthop., 122 (2002), pp. 506-511